Molly Clarke is a writer for the Social Security Disability Help blog, and she approached me about writing an article for my readers who are suffering from severe anxiety disorders that prevent them from working. Knowing how difficult the application process can be, Molly offered her expertise, which you can read below.
Thanks, Molly!
JLS
Anxiety Disorders and Social Security Disability Benefits
Although people tend to think of the term “disability” as a physical impairment, mental and emotional disorders can be just as debilitating. According to the National Institute of Mental Health, one in four Americans suffers from a diagnosable mental disorder.
Anxiety disorders are among the most prevalent of these mental health conditions and can affect a person in a variety of ways. While some individuals with anxiety disorders can live and function normally, others are severely limited by their condition.
If you have an anxiety disorder that prevents you from working and earning a living, you may be eligible for Social Security Disability benefits. Disability benefits can be used to offset lost income, day-to-day expenses, and even medical costs. The following article will provide you with a general understanding of Social Security Disability and will prepare you to begin the disability benefit application process.
SSDI and SSI Technical Eligibility Requirements
The Social Security Administration (SSA) offers two separate types of disability benefits—Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI). Each program offers benefits to different groups of people and each has different technical eligibility requirements.
SSDI benefits are intended to assist disabled workers and their families. Because SSDI is funded by Social Security Disability taxes, eligibility for this program is dependent on applicants’ employment history and previous tax contributions. In many circumstances, applicants are required to have worked and paid taxes for five of the past ten years. However, this changes depending on a person’s age at the time they become disabled. For more information regarding SSDI technical eligibility, click here: http://www.disability-benefits-help.org/ssdi/qualify-for-ssdi.
SSI, on the other hand, is offered to disabled individuals of all ages who earn very little income. Eligibility for SSI is based solely on strict financial limitations put in place by the SSA. SSI benefits are typically the best option for young adults as there are no work history requirements for this program. For more information regarding SSI technical eligibility, visit the following page: http://www.disability-benefits-help.org/ssi/qualify-for-ssi.
Medical Eligibility Requirements
In addition to meeting the Social Security Disability technical requirements, applicants must also meet specific medical requirements. These requirements are published in the SSA’s official manual of disabling conditions—commonly referred to as the blue book. The blue book contains information and medical criteria for many potentially disabling conditions.
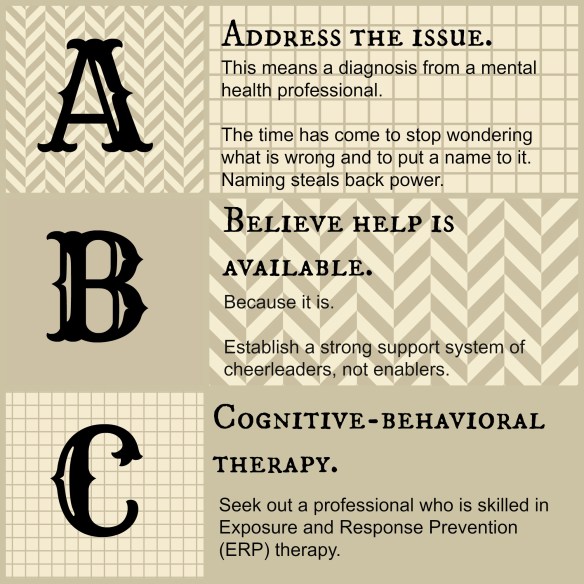
Anxiety disorders are covered under section 12.06 of the SSA’s blue book. To qualify under this listing, applicants must provide medical proof that they experience the following symptoms:
- Persistent anxiety
- Irrational fear of a particular object, activity, or situation
- Severe, recurrent panic attacks
- Recurrent obsessions and/or compulsions
- Intrusive reoccurring memories of traumatic experiences
It is important to note that experiencing the previously mentioned symptoms will not be enough to qualify a person for disability benefits. To qualify for disability benefits, an applicant must experience these symptoms to such an extent that they render the person unable to function in a work setting.
To view this complete blue book listing, visit the following page: http://www.ssa.gov/disability/professionals/bluebook/12.00-MentalDisorders-Adult.htm#12_06
Social Security Disability Application Process
If you meet the technical and medical requirements for Social Security Disability benefits, you can begin the application process online or in person at your local Social Security office. Before doing so, it is in your best interest to collect all required medical and non-medical documents. You can access a list of all required documents on the SSA’s Adult Disability Checklist. (http://www.socialsecurity.gov/disability/Documents/Checklist%20-%20Adult.pdf)
As previously mentioned, once you are ready to apply for benefits, you can completely the application on the SSA’s website or schedule an appointment to complete the application in person at your local Social Security office.
The actual application for benefits consists of several different forms. It is important that you take your time completing these. Provide as much detail as possible when answering questions or submitting information. Doing so will give the SSA insight into how your condition affects your daily life and will prevent delays in the processing of your claim.
Receiving a Decision
After you have submitted your application for disability benefits, it may take several months to receive a decision. While you wait, it is important that you continue with any prescribed medical treatments. You should also save any new or updated medical records that you receive during this time period. Doing so will help you during the appeals process in the event that your claim is denied.
If your application is in fact denied, you will have 60 days in which to appeal this decision. Initially, facing the appeal process may be overwhelming and confusing. However it is important to note that many more applicants are approved during the appeals processes than during the initial application. For this reason, it is important that you do not give up and remain persistent in your efforts.
For more information about Social Security Disability benefits and anxiety disorders, visit Social Security Disability Help (http://www.disability-benefits-help.org/disabling-conditions/anxiety-disorders-and-social-security-disability) or contact Molly Clarke at mac@ssd-help.org.